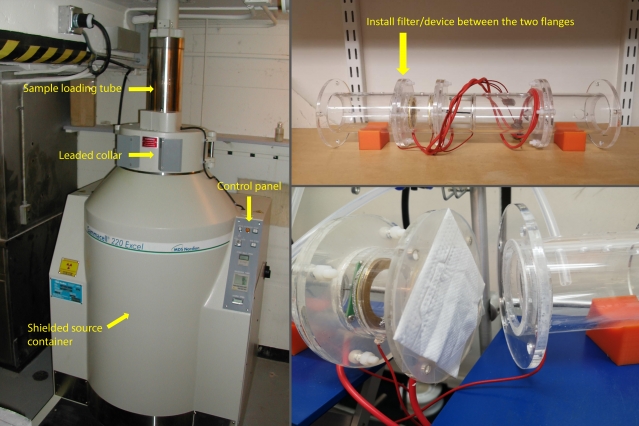
Clockwise from left: Gammacell irradiator in which N95 mask was tested; sodium chloride aerosol apparatus, built by Enze Tian for testing N95 mask filtration efficiency; section of an irradiated N95 mask being loaded into the testing apparatus. Photos courtesy of the researchers.
Nuclear scientists and biomedical researchers, including an HST student, team up to investigate whether treatment with gamma radiation could make N95 masks more reusable.
Leda Zimmerman | Department of Nuclear Science and Engineering
The research described in this article has been published on a preprint server but has not yet been peer-reviewed by scientific or medical experts.
In mid-March, members of the Department of Nuclear Science and Engineering (NSE) joined forces with colleagues in Boston’s medical community to answer a question of critical importance during the Covid-19 pandemic: Can gamma irradiation sterilize disposable N95 masks without diminishing the masks’ effectiveness?
This type of personal protective equipment (PPE), which offers protection against infectious particles like coronavirus-laden aerosols, is in desperately short supply worldwide, and medical professionals in Covid-19 hotspots are already rationing the masks. Gamma radiation is commonly used to sterilize hospital foods and equipment surfaces, as well as much of the public’s food supply, and there has been significant interest in determining if it could allow N95 masks to be reused and address the expanding scarcity.
In a study uploaded on March 28 to medRχiv, the preprint server for health sciences, researchers announced their results: N95 masks subjected to cobalt-60 gamma irradiation for sterilization pass a qualitative fit test but lose a significant degree of filtration efficiency. This form of sterilization compromises the masks’ ability to protect medical providers from Covid-19.
The study, NSE’s first research effort related to the pandemic, also drew on the expertise of MIT’s Office of Environment, Health, and Safety.
“One of our students thought gamma irradiation might be a cool solution to a big problem, and I really wanted it to work,” says Michael Short, the Class of ’42 Associate Professor of Nuclear Science and Engineering, one of the study’s coauthors. “But we quickly recognized that the data went against the hypothesis.”
Team members believe these negative results nevertheless contribute to the larger effort to combat the pandemic. “There has never been a time when negative results are more significant,” notes study lead and co-author Avilash Cramer SM ’18, a fifth-year doctoral candidate in the HST MEMP program, studying radiation physics. Cramer says, “Publishing as quickly as we can means that others working on the same problem can direct their energies in different directions.”
Fast-track research
While they may not have produced the desired outcome, the researchers nevertheless pulled off a study remarkable for its speed and multidisciplinary cooperation — a process inspired and shaped by the immediate threat of the Covid-19 pandemic. “The study took nine days from start to finish,” says Short. “It was the fastest I’ve ever done anything, by orders of magnitude.”
The dire reality of an N95 shortage in the United States sparked widespread concerns early in March. “It had already hit New York, and was on its way to Massachusetts, and President [L. Rafel] Reif wanted to know if we could do something to masks to permit their reuse,” recounts Short. “We looked into different methods, and noticed the idea of using gamma radiation was popping up in a lot of places.”
Cramer was losing sleep worrying about his classmates, medical residents at Boston-area hospitals already in the thick of treating Covid-19 patients. “After reading the literature, it was clear there wasn't a lot of good research out there regarding reusing masks,” he says. “The sky was falling in hospitals with equipment shortages everywhere, and while others had shown gamma rays could inactivate viruses, I wanted to demonstrate one way or the other if they damage the masks themselves.”
N95 masks are manufactured through a variety of proprietary processes using wool, glass particles, and plastics, with 1-2 percent copper and/or zinc. Viewed under a scanning electron microscope, these masks reveal a matrix of fibers with openings of approximately 1 micron. Because the filtering occurs through an electrostatic, rather than mechanical, process, a mask can repel or trap smaller incoming particles. This includes at least 95 percent of airborne particles 0.3 microns or larger in size, such as the airborne droplets that can convey the Covid-19 virus.
A call for multidisciplinary action
On March 11, Cramer emailed several contacts in the radiation physics community in search of a gamma irradiation source. Among the group was Short, who has some experience, among many things, in irradiating plastics. Cramer had worked with Short on previous research ventures, and was familiar with NSE from his time serving as a teaching assistant for an NSE class, Radiation Biophysics (22.055), taught by his PhD advisor, Rajiv Gupta, a physician at Massachusetts General Hospital and an associate professor of radiology at Harvard Medical School.
Short instantly responded to Cramer, offering the campus Cobalt-60 irradiation facility, a source of gamma radiation. “I had an exemption to work on campus and thought, let’s just do it: irradiate and sterilize the masks, then see if they can be used again,” says Short.
With support and guidance from Gupta, also a study co-author, Cramer paused his doctoral work (on low-cost radiology solutions for rural areas), and began writing up a research protocol and drafting additional researchers.
The experiment began on Saturday, March 14, and the first results emerged the next Thursday.
Short gathered the masks from his and a collaborator’s laboratory, keeping a handful for this study before donating the rest (a few hundred) to Beverly Hospital. In Building 6, Short and Mitchell Galanek of MIT Environmental Health and Safety placed the masks into the shielded ring of Cobalt-60, subjecting one group of masks to 10 kilograys (kGy) and another to 50 kGy of gamma radiation (A kilogray is a unit of ionizing radiation). One control group of masks was left unirradiated.
Short then biked the masks to Brigham and Women’s Hospital. There, resident and study co-author Sherry H. Yu, who had signed onto the study after receiving a single emailed invitation, carried out a series of qualitative fit tests. These tests, designed by the U.S. Occupational Safety and Health Administration, establish whether a mask fits securely to someone’s face and screens out potentially harmful aerosolized particles. Yu’s N95 mask-wearing guinea pig was Short himself.
“I spent three hours in a back room at the Brigham in the midst of Covid craziness trying to taste a nebulized sugar solution,” says Short. For this test, saccharin vapor is sprayed into a hood and collar assembly fitted over the head of a subject wearing an N95 mask. By moving their face from side to side and reading a passage, the subject simulates facial movements that might displace or detach the mask and render it less effective. If, after all these motions, a subject cannot taste the sweet mist, the N95 passes. All of Short’s gamma irradiated masks passed the qualitative fit test.
“We thought, Awesome, we’ve done it,” recalls Short. “But colleagues from the Greater Boston biomedical community told us the fit test wasn’t good enough — we needed to assess filter efficiency as well.”
Flawed filtering
Fortunately, the right kind of experimental setup existed just next door at MIT — in the laboratory of Ju Li, Battelle Energy Alliance Professor of Nuclear Science and Engineering and professor of materials science and engineering. Li and doctoral student Enze Tian (both study coauthors) signed on to shepherd the next phase of the study, using an apparatus that shoots sodium chloride particles of different sizes into the N95 masks. The device, normally used to test the protective properties of the Li lab’s masks against tiny metal fragments and nanoparticles, revealed the disappointing results.
“The sterilized masks lost two-thirds of their filtering efficiency, essentially turning N95 into N30 masks,” says Cramer. But why the deterioration?
“Our hypothesis is that ionizing radiation of whatever kind likely decharges the electrostatic filtration of the mask,” says Gupta. “The mechanical filtration of gauze can trap some particles, but radiation interferes with the electrostatic filter’s ability to repel or capture particles of 0.3 microns.”
Gupta is nevertheless pleased by the study’s results. “Even with lowered efficiency, these N95 masks are much better than the surgical masks we use,” he says. “Instead of throwing out N95 masks, they could be sterilized and used as N30 masks for the kind of procedures I do all day long.”
Cramer, who is continuing to explore other N95 mask sterilization methods, believes the study’s results serve a larger purpose: “Adding one more data point to the global understanding of how to clean devices is important — it’s the purest example of the scientific method I’ve ever had the fortune to be part of.”
“Every piece of our hastily assembled machine worked perfectly,” says Short. “We demonstrated that when a crisis hits, scientists can come together for the greater good and do what needs to happen.”
*Originally published in MIT News: https://bit.ly/2JZ88hu