Credit: Image from researchers
Researchers, including an HST faculty member, argue that there is limited evidence of tumor mutational burden as a biomarker of response to immunotherapy.
Mindy Blodgett and Megan Lewis | HST/IMES
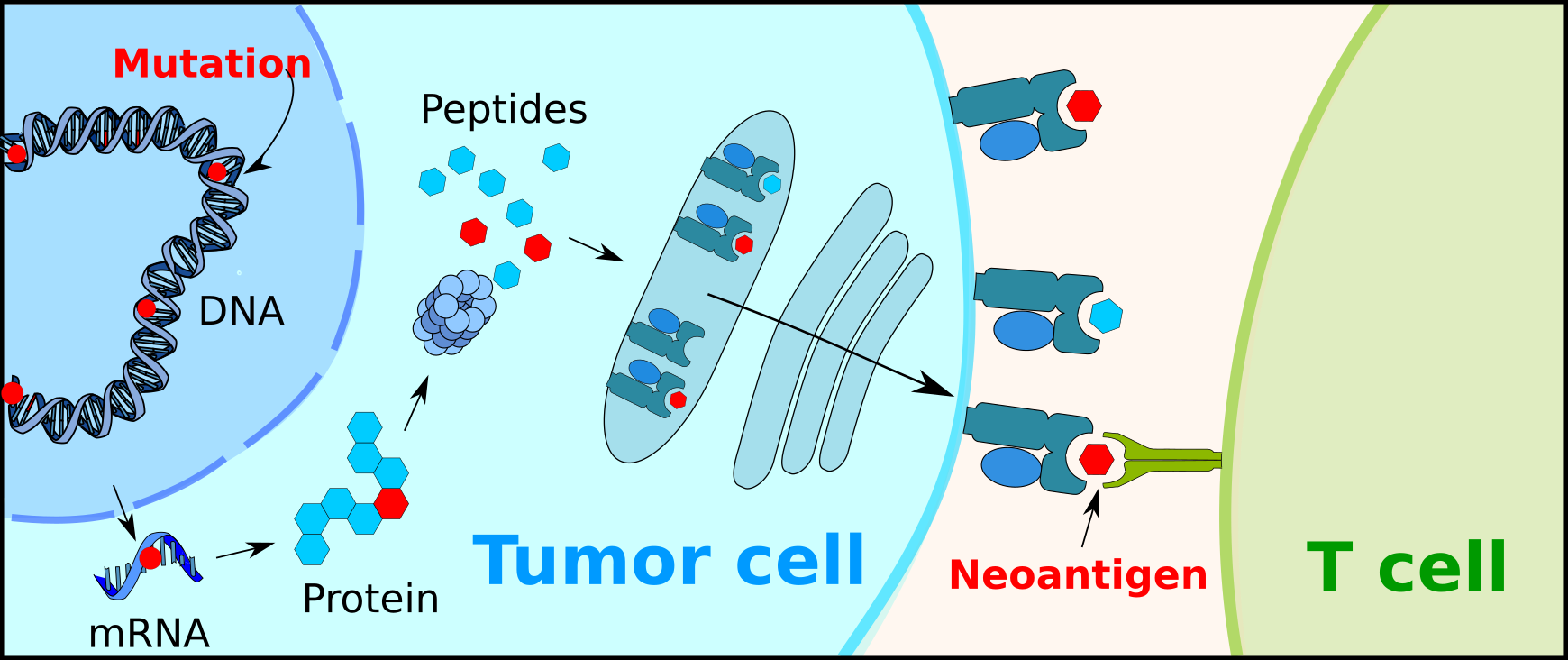
Immunotherapy is an effective cancer treatment, but only for less than half of all patients. This has led researchers to focus on ways to anticipate which patients will benefit most, by examining the number of mutations in cancer—with a belief that the more mutations a cancer has, the more "foreign" it looks to the immune system, and the better the response to the immunotherapy.
Based on a series of high-profile papers published between 2015-2019, which suggested that by using using the "mutational burden" of cancer (the total number of mutations it has) as a biomarker of response to immunotherapy, this approach is now making its way into clinical use, with several companies offering tests to predict if a patient will respond well to immunotherapy. The FDA has recently approved this approach for patient prioritization for immunotherapy.
But recent research by the group of Prof. Leonid A. Mirny, an HST faculty member, and a member of the core faculty at the MIT Institute for Medical Engineering and Science (IMES)—IMES is HST's home at MIT—now challenges this assumption and clinical approach. Mirny recently posted a paper on bioRxiv that revisited the published data and, he says, found no evidence of association between the "mutational burden" of cancer and the clinical response to immunotherapy. After reanalyzing all the data, the Mirny group determined that the original papers had overlooked several cancer-specific aspects of the data, and, in addition, he posits that the statistics had been done incorrectly. Mirny cites his research in saying that if clinicians base treatment decisions on this "mutational burden," in order to decide which patients would most benefit from immunotherapy, then many late-stage melanoma and lung cancer patients might miss out on this life-extending treatment.
Mirny says that the origin of this paper developed completely by chance. As a Qualifying Exam question, Mirny had assigned Joe Luquette, a PhD student in the Bioinformatics and Integrative Genomics (BIG) program at Harvard Medical School (HMS), and now a co-author of this study—to the task of examining the research that supported using the “mutational burden” of cancer to determine which patients would benefit from immunotherapy—and then present the findings. Mirny says he thought it would be a fairly straightforward assignment, but that once he and Luquette, began to examine the data, they made the findings that are now the basis of the paper posted on bioRxiv.
Carino Gurjao, a Bioinformatics Analyst at both Dana-Farber and the Broad Institute of Harvard and MIT, and the first author of the paper, describes how surprised people were when the researchers posted their findings on Twitter: “It became viral. Now we are in the top one percent of research tweets, ever retweeted. It really snowballed out of control and people were really surprised when they (saw our data).”
Mirny says that for cancer patients in the latter stages of cancer, “Their prognosis is really poor without the (immunotherapy) treatment…it’s a question of three to six months survival without treatment. With treatment, many of them can live for years and depriving them of this treatment is really unfair and unjustified.”
The authors are conducting outreach to bring awareness to their research, Mirny says, by contacting medical professionals, the FDA and various cancer advocacy groups, and urging them to consider treating a broader group of patients with immunotherapy.
“We want to encourage that more patients should get treatment,” Mirny says. “It’s a very simple message.”
Mirny says that the response from oncologists, hospitals, and other researchers has been overall positive, and that meetings with entities like the National Brain Tumor Society are planned.
Mirny, and Gurjao—who says he has been presenting the new research to conferences and receiving a positive response—say they have since heard from other researchers who are finding similar results.
In the meantime, Mirny says it was exciting to make such findings due to a question on a qualifying exam, and jokes: “So there is finally some use for (them). It's not only to torture the students!”