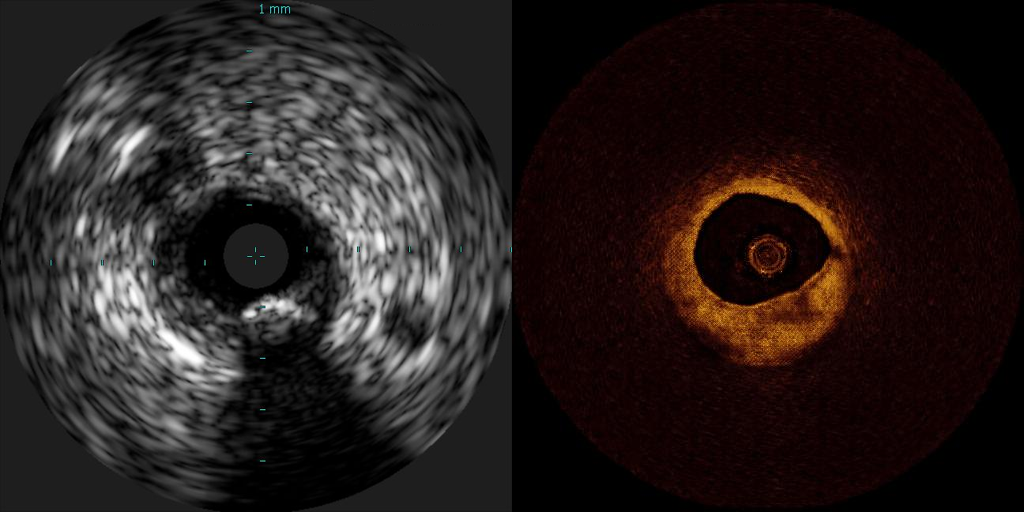
Intravascular imaging (IVUS), on the left, and optical coherence tomography (OCT), on the right (here, a synthetic image generated by artificial intelligence, or AI), are the two main modalities for intravascular imaging for diagnostic purposes. New research uses AI and advanced computational calculations to bridge the gap between these two imaging modalities, providing clinicians with a fuller data set optimizing assessment and treatment strategies.
Credit: Jose M. de la Torre Hernandez and Max Olender
New research from an IMES-based lab shows that AI can be utilized to speed up the process of interpreting intravascular imaging for diagnosis of coronary disease
Megan Lewis and Mindy Blodgett | IMES
Intravascular imaging is a useful catheter-based system giving physicians images of diseased vessels deep inside the body. But it is an invasive form of managing coronary disease, requiring specialized training. Now, researchers, including at IMES, have utilized artificial intelligence (AI), to devise a new way of incorporating the technology into the process of diagnosis, facilitating and speeding up interpretation in real-time.
Max Olender, a scholar in the Graduate Education in Medical Sciences (GEMS) Certificate program, and a postdoctoral associate in the Edelman Lab at the MIT Institute for Medical Engineering and Science (IMES), which is also known as the Harvard-MIT Biomedical Engineering Center, has led the groundbreaking research focused on AI in medicine. Elazer R. Edelman, the Edward J. Poitras Professor in Medical Engineering and Science at MIT, the director of the lab, also directs IMES and is cardiologist at the Brigham and Women’s Hospital (BWH) in Boston. IMES is HST's home at MIT.
The new research, “Artificially synthesized optical coherence tomography images based on intravascular ultrasound-virtual histology examination of diseased coronary artery”, has appeared on PCROnline (which is supported by EuroIntervention journal), one of most prestigious platforms of cardiovascular intervention. It has also appeared in the European Health Journal — Digital Health.
Medical imaging provides clinicians with visual representations of a patient’s interior body. These visual representations are shown based on how the specific tissue interacts with the imaging system (e.g., how tissue responds to mechanical vibrations in an ultrasound).
Based on this medical knowledge, Olender explains that if the “distribution of tissue in the physical system is known, a corresponding medical image can be generated for any image type for which the tissue’s interaction with the imaging system is understood.”
He further explains that since “tissue behavior can be very complex and difficult to describe mathematically,” he and his team devised the new approach of incorporating AI into diagnosis, which “provides a convenient and effective means to learn these relationships and produce medical images of tissue distributions”. In doing so, they created an innovative system for synthetic intravascular imaging, a technology used in diagnosing and treating coronary artery disease and other atherosclerotic disease.
Olender explains how the AI technology approach works: “The system studies the relationship between structure and appearance of arteries (blood vessels). It’s shown many images and told what it’s looking at—the vessel’s geometry and distribution of different tissue types.
The goal of this new approach is to use AI technology to expedite and ease access to the best available information for cardiologists to use when interpreting results and seeking a diagnosis. By using AI in this manner, the cardiologist can access information faster, without being overwhelmed or needing to review each individual source of information. The hope is that this will increase the speed and accuracy of diagnosis, prognosis and decision-making during vascular interventions.
“Based on the relationships it learns,” Olender continues, “the system creates images that would be expected for any given vessel structure. Through iterative training, the system achieves increasing accuracy and realism.”
Olender says that this new approach can be applied in multiple ways, including as a means to “translate” between imaging system types. This facilitates interpretation by doctors who may be more familiar or comfortable with a type of imaging other than the type which was acquired.
Olender explains how the technology can be used to integrate multiple sources information into a single intuitive image: “Different imaging systems and tests have different strengths and weaknesses in distinguishing tissue structure. Information about the physical system that is derived from each can be combined, taking advantage of the benefits of each, then expressed by this system in a familiar image.”
Dr. Eyal Ben-Assa is an interventional cardiologist in Israel who completed his interventional cardiology fellowship at Massachusetts General Hospital. He is a user of intravascular imaging and enthusiastic about the prospects for synthetic imaging in the field.
He says that in general, intravascular imaging is beneficial, in that it allows cardiologists to advance a miniaturized imaging probe through the artery of the hand to the coronary arteries of the heart, and directly image pathologic atherosclerotic narrowing that may cause myocardial injury.
“Acquiring these images allows us to diagnose and to guide interventional procedures to treat correctly the diseased vessel,” he says.
Currently, the two main modalities for intravascular imaging are intravascular ultrasound (IVUS) and optical coherence tomography (OCT). While both have been developed and improved over the past three decades, they are different with very distinct characteristics.
Dr. Ben-Assa describes these differences: “While IVUS has a relatively low resolution of 100 μm it has a high tissue penetration that allows assessing the entire structure of the coronary artery, whereas OCT has a higher resolution of 10–20 μm (or, millionths of a meter) allowing direct assessment of fine endoluminal structures yet with a limited tissue penetration compared to IVUS.”
He applauds the new research, saying that “In a series of studies performed in relatively short period, (the research) was able to use advanced computational calculations and artificial intelligence to bridge the gap between these different imaging modalities and allowed a significant leap in the field.”
The developed software, based on AI, processes data from IVUS images to artificially synthesize OCT images, thus enabling clinicians to review all the data they need in a single imaging procedure, in their preferred style of reviewing.
“As an interventional cardiologist, I use intravascular imaging on a weekly basis,” says Dr. Ben-Assa. “Although its use has been correlated with improved clinical outcome in certain scenarios, the adoption rate of intra vascular imaging is still relatively low, for reasons of costs, lengthening of the procedure, will to minimize contrast media use and the need to choose between two different imaging modalities.”
He explains how Olender’s new research may alleviate some of the aforementioned issues by “allowing for rapid, comprehensive evaluation of atherosclerotic lesions while minimizing adverse events.
“The operator will get the full data set that will allow for full plaque morphology assessment and optimize our treatment strategies.” The research can lead to clinicians being able to acquire a full data set allowing for a full assessment, optimizing treatment strategies, according to Ben-Assa, and it has the potential “to change the way we treat coronary arteries.”