“We're looking at things ranging from gene editing in the lungs to immunotherapy and thinking about new cancer treatments,” Sayo Eweje says.
Credits:
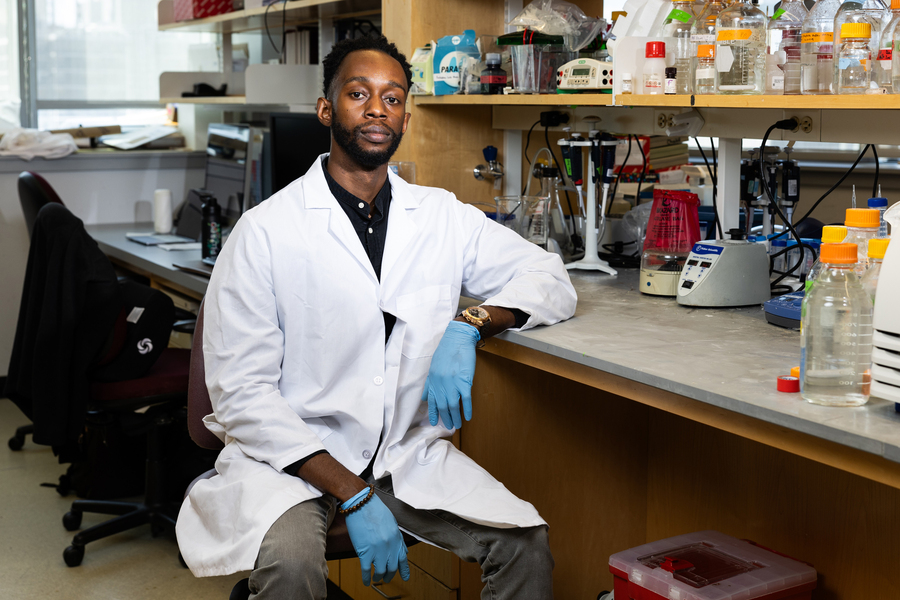
Photo: Jake Belcher
HST MD/PhD student Sayo Eweje seeks to develop new technologies for delivering RNA and protein therapies directly to the body’s cells.
Austin Chen | MIT News correspondent
Early in his undergraduate studies in bioengineering, Sayo Eweje was thinking of a career in medicine. He was inspired by the idea of harnessing medical knowledge to improve patients’ lives, having grown up seeing his father do so as a gastroenterologist. However, his research experiences in college made him appreciate how scientific advancement can lead to paradigm-shifting innovations. What if he could contribute to breakthroughs that improved lives on a much larger scale?
“That idea really captured me, and I realized that we’re only enabled to do that by really delving into the frontiers of science,” he says. In his junior year of college, he decided to aim for a career as a physician-scientist, splitting his time between caring for patients and conducting research. After graduating, he entered the Harvard-MIT MD/PhD program, which is affiliated with both Harvard Medical School and MIT’s Institute for Medical Engineering and Sciences (IMES).
Now, Eweje is entering his sixth year in the program, and the fourth year of his PhD studies in medical engineering and medical physics (MEMP) through the Harvard-MIT Program in Health Sciences and Technology. Throughout his PhD, he has worked in the lab of Elliot Chaikof at Beth Israel Deaconess Medical Center, where his research has focused on the development of protein-based nanoparticle systems for delivering nucleic acid and protein therapies directly to cells inside the body.

Eweje intends to continue encouraging young people to explore STEM. “Everyone should have the right to explore their fullest potential,” he says.
Photo: Jake Belcher
Eweje’s interest in this area was sparked shortly after he entered the program: Initial reports describing a promising new gene editing-based treatment for inherited blood disorders were released, highlighting the curative potential of this approach. However, administering this therapy involves removing blood-forming stem cells from patients, editing them, then putting them back in. In order to accommodate the edited cells, recipients undergo heavy chemotherapy, which led to questions surrounding toxicity and scalability.
“The thought that I had, and that many others in the field had, is that if we could deliver these gene-editing therapies inside of the body without having to remove cells, without having to do this chemotherapy, his could be a much more effective and accessible therapy,” Eweje says.
“After thinking about problems like that and understanding that a lot of this ultimately comes down to drug delivery and engineering nanoparticles and delivery vehicles, I realized that’s where I want to spend my time,” he says. “There are so many challenges in treating disease where the bottleneck ultimately comes down to effective delivery.”
Striking disease at the source
A number of diseases are caused by mutations in hematopoietic (blood-forming) stem cells, and Eweje chose Chaikof’s lab in part because the team was looking for ways to deliver RNA and protein therapies directly to those cells in patients. The work has spun off in many interesting directions since then.
“It started there, but it has become a much broader platform-focused project,” Eweje explains. “We’re looking at things ranging from gene editing in the lungs to immunotherapy and thinking about new cancer treatments.”
This January, he published an article in Biomaterials that gave a progress update on the state of research using protein-based nanoparticles to deliver nucleic acid therapies to cells. Historically, scientists have found success with viral vectors for delivering gene-based therapies, but because of those viral origins, there remains the possibility of triggering a patient’s immune system.
“Protein materials, particularly human-derived protein materials, are far less likely to trigger that immune response, which is one major advantage,” he says. “The other thing that we’re actively working towards in the lab is this idea of leveraging programmability and precise structure in recombinant proteins.”
While much work remains to determine whether nonviral, protein-based nanoparticles can used as effectively as those that are virus-derived, or lipid nanoparticles, he’s grateful to have learned valuable lessons during this process.
“I really appreciate the fact that I’ve had an opportunity to learn about what’s out there, better understand the challenges, and carry that knowledge forward,” he says.
Building opportunity for others
Outside the lab and the hospital, Eweje is engaged in education and outreach projects as close as Cambridge and as far as Nigeria, where his family traces their roots. He is a co-founder of the Program of Ragon and IMES in Science and Medicine (PRISM), which hosts weekly programs for high school students in the greater Boston area to learn directly from scientists and clinicians about various topics in STEM.
“I see kids as stem cells,” he says. “They have so much potential to differentiate into so many different things, but you have to put them in a proper environment and give them the exposure required to understand where they can go.”
He’s also a co-managing director of the Critical Healthcare Information Integration Network (CHIIN), a nonprofit that provides medical information to community health workers in rural and underdeveloped areas of Africa. It operates via a chatbot that can respond to queries over SMS text messaging and is therefore able to reach communities without internet access, indirectly assisting thousands of patients.
“Part of it was developing confidence in the users by giving them something to have in their back pocket as a reference tool,” he says.
As his time in the HST program draws to a close, Eweje aims to defend his PhD next year and return to full-time clinical work at Harvard Medical School. Ultimately, he envisions a career at the intersection of clinical medicine and biotech innovation.
He also intends to continue encouraging young people to explore STEM. “Everyone should have the right to explore their fullest potential,” he says.
“I find a lot of gratification in the impact that we can have on someone’s life just by giving them the opportunity to learn about something, which could change the trajectory of what they do,” he adds. “We have not only the pleasure of doing that, but also a little bit of an obligation.”
*Originally published in MIT News.